Anatomy & Physiology: Joints—Ligaments.
Structure.
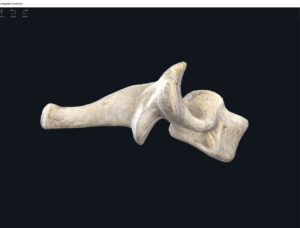
Shoulder.
- Articular capsule: thin loose sac lining that encompasses all the shoulder joint structures—glenoid cavity to anatomic neck of humerus.
- Coracohumeral ligament: ligament that runs from the coracoid process (scapula) to greater tubercle (humerus). It lies deep to the subacromial bursa, the coracoacromial ligament.
- Glenohumeral ligaments: 3 ligamentous bundles anterior and deep to the subacromial bursa and coracoacromial ligament. They run from the glenoid cavity to the lesser tubercle and anatomical neck of humerus. Stabilize shoulder near endpoints of ROM.
- Glenoid labrum: narrow strip of fibrocartilage around the perimeters of the glenoid cavity that provides a little deeper and more surface area for the socket.
- Bursae: reduce friction. There are 4: subscapular, subdeltoid, subacromial, and subcoracoid bursa.
- Acromioclavicular ligament.
- Coracoacromial ligament.
- Transverse humeral ligament.
- Coracoclavicular ligament.
- Conoid ligament.
- Trapezoid ligament.
- Superior transverse scapular ligament.
Elbow.
- Articular capsule: from humerus to ulna and anular ligament.
- Anular ligament: around the head of the radius. Posteriorly runs from capitulum, olecranon fossa, and lateral epicondyle of humerus; to anular ligament of radius, olecranon of ulna, and ulnar posterior and radial notch..
- Ulnar collateral ligament: from medial epicondyle of humerus to coronoid proces and olecranon of ulna.
- Radial collateral ligament: runs from lateral epicondyle of humerus to anular ligament of radius and ulnar radial notch.
- Anular ligament of radius: encircles radial head to help hold the radial head to ulnar radial notch.
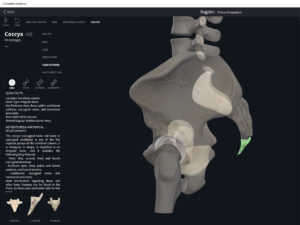
Hip.
- Articular capsule: dense and strong; extending from edge of acetabulum to femoral neck. Articular capsule is strengthened by the bidirectional fibers: circular fibers zona orbicularis (like a collar around the neck); and longitudinal fibers.
- Iliofemoral ligament: runs from ilium of hip to intertrochanteric line of femur.
- Pubofemoral ligament: the part of the articular capsule that runs from the ischial wall of the acetabulum to femoral neck. Slacks: adduction. Tenses: abduction. Reinforces articular capsule.
- Ligament of femoral head: runs from the fossa of acetabulum to fovea capitis of femoral head.
- Acetabular labrum: a fibrocartilage rim around acetabulum to increase the depth and surface area of the hip socket to the head of femur can articulate.
- Transverse ligament of acetabulum: crosses over the inferior acetabulum and connects with ligament of femoral head and articular capsule.
Knee.
- Articular capsule.
- Medial and lateral patellar retinacula: fused band of tendons at the quadriceps femoris muscle and fascia lata (deep fascia) of thigh. Reinforces anterior of joint.
- Patellar ligament: from the tendon of quad femoris extending from the patella to tibial tuberosity. The infrapatellar fat pad separates this ligament from the synovial membrane.
- Oblique popliteal ligament: from lateral condyle of femur to head and medial tibial condyles. Reinforces posterior of joint.
- Arcuate popliteal ligament: from lateral condyle of femur to fibular head. Reinforces posterior of joint.
- Tibial collateral ligament: from the femoral medial condyle to tibial medial condyle. Reinforces medial area of joint. Attaches to menisus as well.
- Fibular collateral ligament: runs from femoral lateral condyle to fibular head. Reinforces lateral area of joint.
- Intracapsular ligaments: located within articular capsule; runs from femur to tibia.
- Cruciate ligaments (anterior and posterior): attached to tibia and cross over each other to the femural end.
- Anterior cruciate ligament: runs from posterior to lateral; from the anterior tibial intercondylar area to the femoral medial surface of the lateral condyle. ACL limits ROM hyperextension and prevents anterior sliding dislocations.
- Posterior cruciate ligament: runs from tibial posterior intercondylar area to femoral lateral area of medial condyle. Prevents sliding dislocations upon knee flexion.
- Articular discs (menisci): 2 discs made of fibrocartilage to pad out the bones.
- Medial meniscus.
- Lateral meniscus.
- Bursae.
Function.
Clinical Significance.
- Rotator cuff injury: usually a strain/tear of the rotator cuff muscles (esp. supraspinatus tendon).
- Dislocated shoulder: usually results from the displacement of the head of the humerus (usually inferiorly).
- Separated shoulder: usually where the scapular acromion is displaced from the clavicular acromial end from some kind of blow to that area or fall.
- Torn glenoid labrum: when the fibrocartilaginous labrum tears away from the glenoid cavity.
References
Biel, A. (2015). Trail guide to the body: A hands-on guide to locating muscles, bones and more.
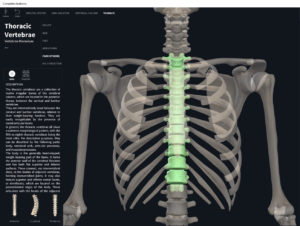
Cedars-Sinai. (2018). Vertebrae of the spine. Retrieved from https://www.cedars-sinai.org/health-library/diseases-and-conditions/v/vertebrae-of-the-spine.html
Jenkins, G., & Tortora, G. J. (2012). Anatomy and Physiology: From Science to Life, 3rd Edition International Stu. John Wiley & Sons.
Muscolino, J. E. (2017). The muscular system manual: The skeletal muscles of the human body.